This is a OPINION PIECE and should be interpreted with CAUTION!
The text is ‘overtly simplified’ for general audience and DOES NOT CLAIM scientific accuracy but is only intended to present easy to understand information.
first published: 24.11.2020
Context: In scientific literature as well as in common news media, there are scattered reports of SARS-CoV-2 ‘reinfection’, mostly experiencing asymptomatic or mild symptoms during the first infection. Meanwhile, there are also reports accumulating for people with prolonged SARS-CoV-2 symptoms, some reporting up to several months since the first diagnosis, and sometimes termed as ‘long-COVID’. Both are clinical manifestations following the SARS-CoV-2 infection and is not well understood at present, partly because the immunology of asymptomatic individuals or symptomatic individuals with mild symptoms (no hospitalization required) is not a priority at the moment.
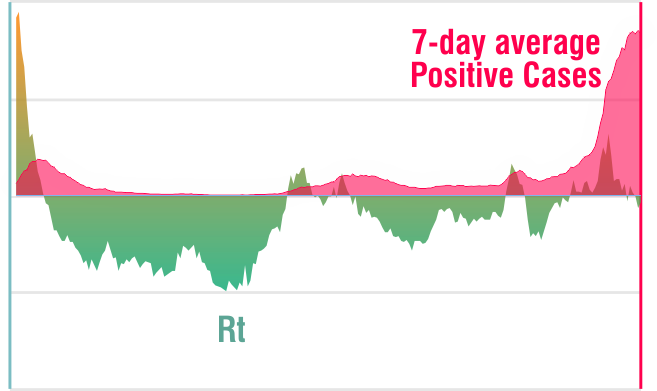
Observations and Hypothesis: Initial studies show a wide range of SARS-CoV-2 ‘viral-shedding‘ in infected individuals, from a few days to up to several weeks. Although the mechanistic details are unclear, the fact remains that certain proportion of population (probably a small minority) is experiencing a longer period of ‘viral shedding’ (a prolonged period of viral clearance). In principle, such individuals pose a higher risk for themselves (in case of mild- to medium-symptoms, would experience ‘long-COVID’) and others (in case of asymptomatic cases, may infect others without knowing it). In effect, it would mean that a ‘small’ fraction of recovered cases, with or without symptoms (mild-disease), who are able to socialize after 10-14 days of ‘quarantine-period’ BUT without a confirmatory SARS-CoV-2 negative PCR test, has the hallmarks of prolongling the pandemic.
Coming back to the possibility of a ‘reinfection’, there are probably two major possibilities. First, it is not a ‘true reinfection’ and rather a ‘recurrence or reactivation’ of the primary infection following a waning immune respose and the virus can propagate again. It may be argued that the antibodies are not sufficient to avoid a ‘recurrence or reactivation’ of the infection, it should be appreciated and noted that even if a suboptimal response, antibodies protect against developing severe forms of the COVID-19 disease in these individuals (for severe COVID-19, see section below). The second possibility could be a ‘true reinfection’, which would clinically mean that an another strain of the SARS-CoV-2 infecting an individual for a second time, which could not be recognized by the immune response developed during the first infection. The second possibility although has a very small probability, if true, would have large implications on vaccine development and ‘herd-immunity’.
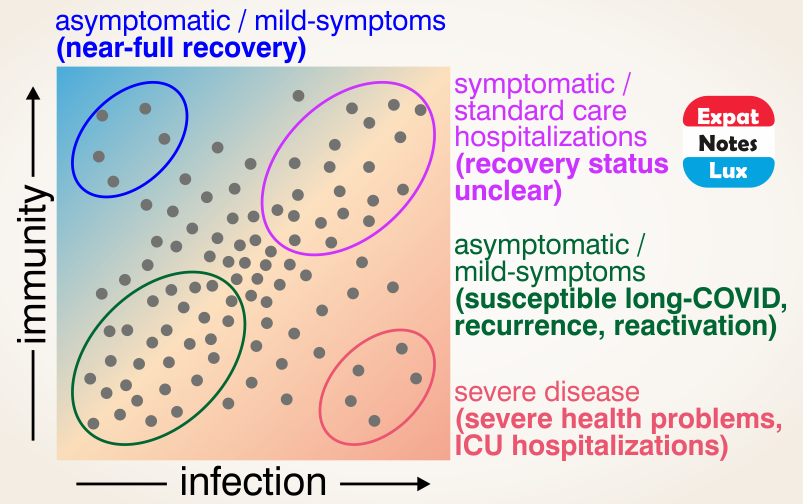
It may also be important to mention that in case of severe COVID-19 disease, comorbidities (like cardiovascular disease, diabetes and obesity, are most common), immunocompromised or immunosuppressed individuals, age (old versus young), gender (male and female) and genetic factors (like blood groups) also play a role, further complicating a simple and universal solution like a ‘single type’ of vaccine for everyone.
In summary, the individual immune responses during SARS-CoV-2 infection or COVID-19 desease remains varied and largely unknown, and probably the acquired immunity following vaccination would also vary a lot amongst individuals, and consequently further caution in terms of re-opening activities with large gatherings, maintaining interpersonal distance, hygiene measures and post-recovery PCR tests are warranted.